What is Knee Replacement Surgery?
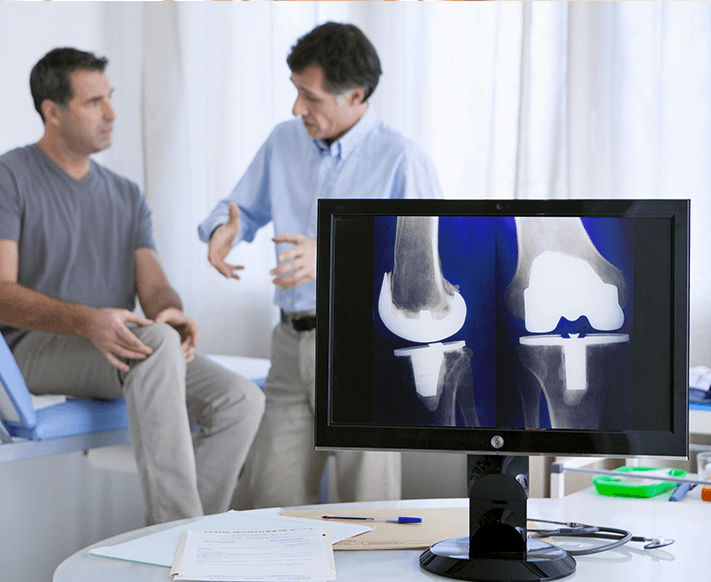
Knee replacement surgery, also known as knee arthroplasty, is a medical procedure in which a damaged or diseased knee joint is replaced with an artificial implant. This surgery is typically performed to relieve pain and restore function in individuals with severe knee arthritis or other debilitating knee conditions. The procedure involves removing damaged cartilage and bone from the knee joint and replacing them with prosthetic components made of metal, plastic, or ceramic materials.
When is Knee Replacement Surgery Needed?
Knee replacement is typically considered when:
Pain and stiffness in the knee significantly affect daily activities such as walking, climbing stairs, or getting up from a chair
Conservative treatments, including physiotherapy, medications, and injections, no longer provide relief
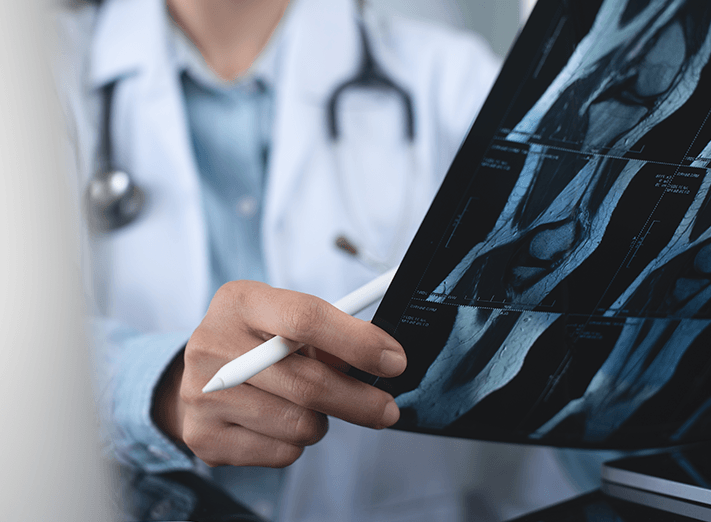
There is severe joint damage seen on X-rays or MRI scans", "The knee is deformed or unstable, making movement difficult
The patient’s quality of life is significantly reduced due to knee pain