What Is Plantar Fasciitis?
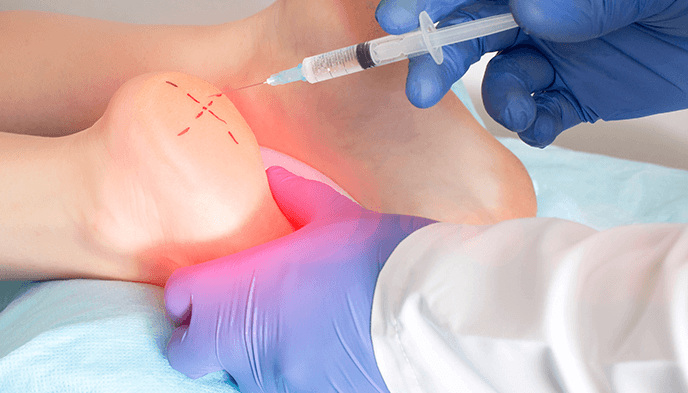
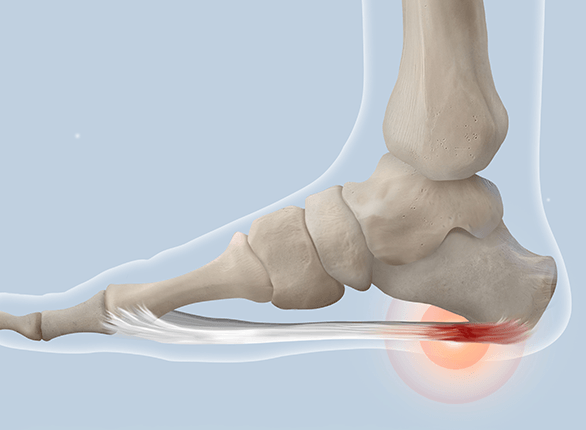
Plantar fasciitis is a common foot condition that causes pain and inflammation in the plantar fascia, a thick band of tissue that runs along the bottom of the foot from the heel to the toes. This condition occurs when the plantar fascia becomes irritated or strained due to excessive pressure, repetitive stress, or improper foot mechanics. It is one of the leading causes of heel pain and can affect people of all ages, though it is most common in runners and individuals who spend long hours standing.